Written by TMRnerve.com Staff
According to David A. Brown, MD, FACS, nearly 95% of patients who undergo amputation report chronic pain. He says the pain can be “quite severe” and it usually feels like “residual limb” pain, which is early in the amputation healing and “phantom pain” which is mostly felt later in recovery and can last indefinitely. TMR nerve surgery aims to reduce that pain.
Brown, an Assistant Professor of Surgery, as well as Director of Duke Wound Management Clinic, says, “We don’t really know how the quality of pain changes after TMR surgery, but global pain scores decrease. We rely on what patients report, which is that the perception of pain or the quality of the pain changes.”
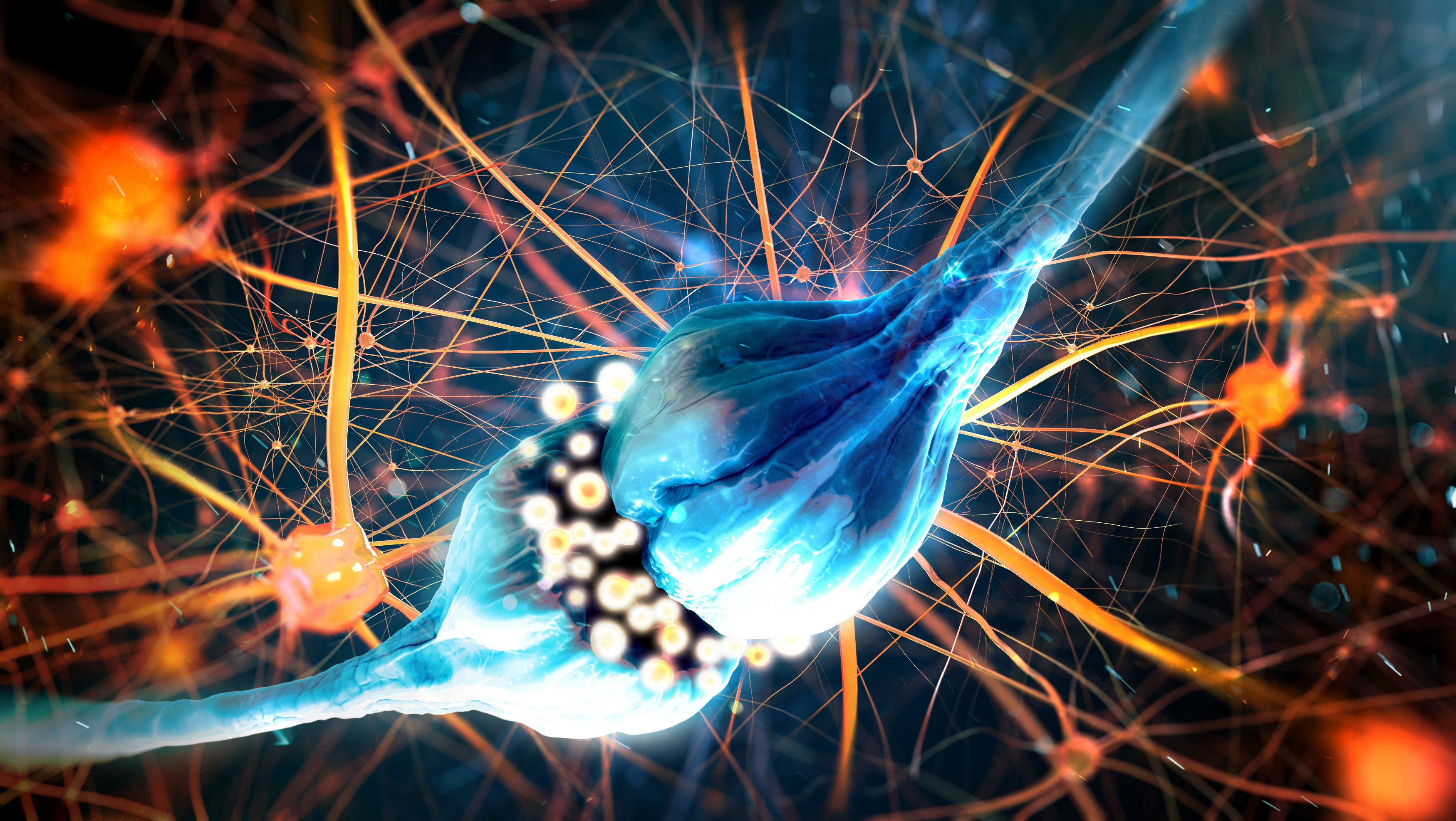
How do we understand pain? Imagine you had a right-hand injury. The pain signal coming from the site of injury will travel up to the brain, and this is where the awareness of pain essentially is felt. When a body part is injured, various chemicals are released into the area around it. These chemicals irritate the pain nerve endings sending a message towards the spinal cord and then onto the brain. (1)
After an amputation, due to the body’s natural reaction to injury, there can be changes at multiple levels in how pain is experienced. The injury, or “pathology”, of amputation causes changes to happen at the area where nerves are cut, and also to the spinal cord, and the brain. At the area around the nerve, there is increased awareness of feelings inside and outside of the body like adrenaline or any motion or touch of hot or cold.
The brain and spinal cord normally receive a high amount of communication, basically traveling through the nerves and connecting nerves to the brain naturally, from the limbs. After a major limb amputation, this communication or connection is gone. The neurons - cells that communicate with nerves - desperately seek new connections, which causes some cross-wiring or confusion in the nerves and the sensation of pain. This explains why patients with phantom limb pain (pain that feels like it's coming from a body part that's no longer there) (2) can be triggered by areas around the amputated limb.
An example of this in leg amputations is when phantoms are felt during urination because the brain’s “maps” of sensation of the genitals and the leg are near each other. Dr. Brown reports, “I’ve seen patients where that goes away after TMR surgery. But everything starts with the cutting across of the nerves. That starts the whole series of events. This is why we think the best option is to do TMR at the time of amputation. It stops some of that abnormal feedback, and we hope to halt or even reverse the pathologic changes in the brain.”
Usually patients with the greatest benefits from TMR are those who get the surgery at the time of, or soon after amputation. This is to avoid the pain of the limb loss before its starts, by rewiring the nerves. This is why TMR can reduce or reverse some of the ways pain is felt, because the nerves are rewired by being surgically reconnected to nearby nerves and, eventually, muscles. If you think about nerves as electrical wiring, TMR helps to complete the circuit by reconnecting the live wire.
So why is TMR surgery not a standard part of amputation protocol? Dr. Brown reports, “In the science of amputation, TMR has only been around for about 10 years, and only five or so in mainstream surgical practice. It requires a collaborative effort among surgeons: plastic surgeons have performed the majority of TMR procedures, whereas vascular or orthopedic surgeons typically do the actual amputation."
While a number of therapies exist to manage post-amputation pain, Targeted Muscle Reinnervation (TMR) is a surgical treatment quickly gaining acceptance as a treatment for nerve pain associated with amputation.
To learn more, visit Is TMR Right for Me?
Reference
Written by TMRnerve.com Staff
Targeted Muscle Reinnervation (TMR) is a surgical treatment that is gaining acceptance for nerve pain associated with amputation.
TMR is not a treatment option for patients with spinal cord injuries, brachial plexus injuries, or who are generally not healthy enough for surgery. The procedure does present typical risks of surgery. Patients may experience a temporary increase in pain as part of the nerve healing process. Your physician will help you determine whether TMR is right for you.
Gregory Dumanian, MD, is medical director of TMRnerve.com. He is a paid consultant of Checkpoint Surgical, Inc.
Copyright Checkpoint Surgical, Inc. 2025 Privacy Policy